A report in VeloNews on the eve of the Tour de France stated that the French government had insisted that the “two strikes and you are out” policy must be enforced by the ASO. This means that if two positive COVID-19 test arise within a team or its support staff, the team will be removed from the race. This raises the possibility of the yellow jersey rider being ejected from the race if, for example, two mechanics record positive tests. This would be particularly unjust if it turns out that a test result was a false positive. So what are the chances that this might happen?
False positives
One of the great frustrations of the reporting on COVID testing has been the lack of clarity about what type of testing is being discussed. Tests fall in to two categories. Antigen tests use a sample from a nasal or pharyngeal swab to detect patients who currently have the disease, whereas antibody tests use a blood sample to identify patients who have developed antibodies as a result of exposure to the disease in the past – more than 28 days earlier.
There are two general types of antigen test. Real time polymerase chain reaction (RT-PCR) tests looks for specific viral fragments and need to be conducted in a laboratory, typically requiring at least 24 hours for a result. Less reliable rapid tests look for proteins associated with the COVID-19 virus, producing results in as little as 15 minutes.
The UCI requires riders and staff to be tested using RT-PCR, which is a very reliable method, having both high sensitivity (ability to detect those with the disease) and high specificity (ability to clear those without the disease). The relevant question for the Tour de France is the probability of a false positive RT-PRC test. Indeed Larry Warbass recently said he thought his result was a false positive, as he had experienced no symptoms and had maintained strict self isolation during training.
The evidence indicates that the machines performing the RT-PRC test are extremely unlikely to generate a false positive, because the test needs to find significant levels of three different targets to confirm the presence of COVID-19. In FDA experiments, 100% of negatives where correctly identified – there were no false positives. However, it remains possible that, in the moving circus of the Tour de France, a sample could become contaminated before it is tested or that samples might somehow be mislabelled. A high level of responsibility falls on the shoulders of team doctors to minimise these risks, but we can never be sure that it is zero.
One in a thousand
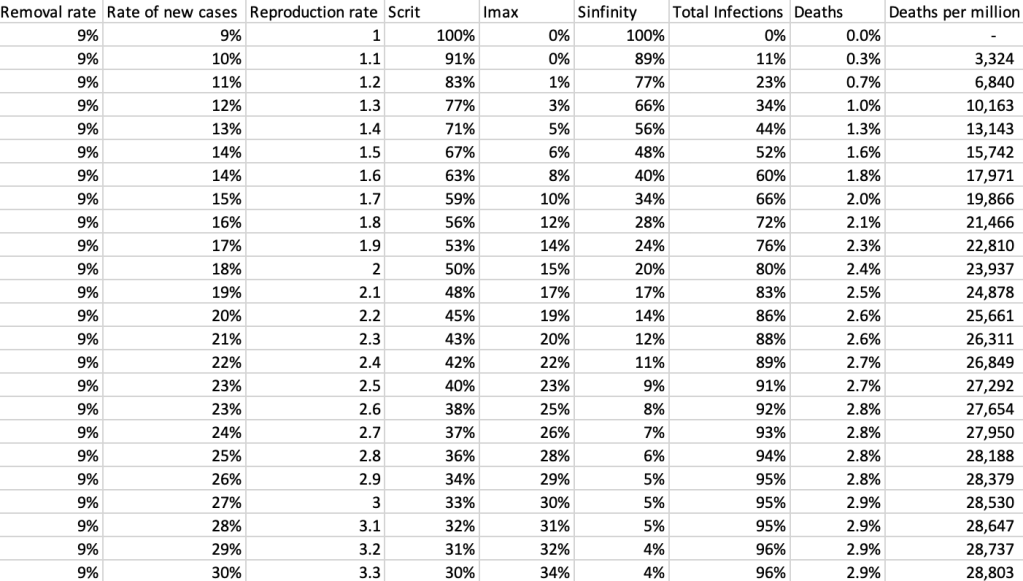
As a thought experiment, suppose that a negative RT-PCR test is 99.9% reliable, i.e. that one COVID-free person in a thousand somehow produces a false positive result. What is the chance that a team is unjustly sent home from the Tour?
Each team has eight riders plus support staff. Although teams might want to reduce the number of staff in the team bubble, it may be necessary to have extra catering staff in order to remain self sufficient. Let us assume an average of 17 staff on each of the 21 teams and that everybody has passed the required two negative tests prior to the start of the race. Assume further that nobody contracts COVID-19 throughout the race.
It has been indicated that everyone will be tested on the two rest days. Reassuringly, the probability of two or more false positives in a single team bubble of 25 people would be 0.03% (1-0.999^(25*2)). However, the probability that every team rider receives a negative result would be only 85% (0.999^168), meaning that there would be a 15% chance that at least one rider is unjustly ejected from the race. In fact, since at total of 1,050 tests would be taken by everyone in a team bubble, the chance of at least one person receiving a false positive would be surprisingly high: 65% (1- 0.999^1050).
Perhaps the assumption of 1 in a thousand false positives was a bit alarmist. Reducing it to 1 in thousand still produces a probability of 10% that somebody would be sent home during the Tour.
Blind eyes
In some situations, draconian sanctions might deter team members or staff from reporting symptoms. One could imagine a soigneur or mechanic having to go home quietly after mysteriously spraining a wrist. However, this could create very negative press coverage if word got out that this person was infected.
Furthermore, the UCI rules place responsibility on the teams and specifically the team doctors to apply strict daily monitoring and controls to detect suspected COVID-19 cases.
Champs Elysées
While in the above scenarios no one actually contracted COVID-19, there is, of course a not inconsiderable chance that one of the 525 people in the team bubbles does actually become infected. If the virus spreads to more than one team, the whole race could become a fiasco.
But let’s keep our fingers crossed and hope Tour makes it to the Champs Elysées.